de Mola, J. Ricardo Loret; Carpenter, Sue E.
|
|
|
Chief Editor’s Note: This article is the 11th of 36 that will be published in 1996 for which a total of up to 36 Category 1 CME credits can be earned. |
|
HISTORICAL OVERVIEW
|
|
The first reports of genital prolapse are those of the Ebers papyrus, dated 1500 BC. No discussion regarding possible causes was made, but the suggested treatment was to smear the fallen womb with a mixture containing honey and subsequent replacement. Hippocrates (400 BC) mentioned genital prolapse in his writings and described three methods of treatment. The first was by tying the patient to a ladder that was then turned upside-down and shaken violently hoping to reduce the uterus. He also described the placement of suction cups to the buttocks and lower abdomen expecting to replace the prolapse. A third option described was sponing the prolapse with cold wine, raising the foot of the bed until the uterus was completely reduced, then it was supported in position by a half pomegranate soaked in wine and introduced into the vagina. This was the first time that the concept of a vaginal pessary was used in the management of genital prolapse. Celsus (25 BC) and Soranus of Ephesus (98 AD) used a very similar method of treatment, where the prolapse was washed with an astringent lotion and manual reduction of tissues into proper place, followed by the introduction of a medicated pessary into the vagina and binding the legs firmly together. Aretaeus (100 AD) and Galen (130 AD) believed that the prolapse was able to reduce itself and used fumigations to promote this. Haby Abbas (932 AD), a well-known Persian physician, wrote extensively about genital prolapse. He described prolapse as a condition that was related to birth trauma and managed the prolapse by cleaning, manual reduction, introduction of a wool pessary and binding the legs together. Later Caspar Stromayr of Lindau recommended the use of tightly rolled sponges dipped in wax and covered with oil or butter as pessaries Figure 1 and Figure 2. This was the accepted mode of treatment for hundreds of years, until the first surgical methods of treatment appeared in the 1800s when Donald of Manchester and his assistant, Fothergill, described what became known as the Manchester operation for the treatment of genital prolapse [1]. |
|
|
The first case of genital prolapse in a newborn was reported by Conovius in 1723 [2]. The first formal review on the condition was written in 1897 by Ballantyne and Thomson [3], where they reported the autopsy findings of two neonates who presented with spina bifida and genital prolapse and reviewed the six previously reported cases. They also described a possible pathophysiology, suggesting that disturbances in the innervation of the genital area secondary to spina bifida were responsible for this condition. Findley [4], in 1917, found that prolapse of the uterus in the newborn and nulliparous women constituted 3.45 percent to 13.15 percent of all cases of prolapse and of these, 82 to 86 percent of cases were associated with spina bifida. He also described several cases of procidentia that occurred about the time of puberty, where the girls were poorly nourished, some had pulmonary tuberculosis associated with persistent coughing, and others were simply involved in hard labor duties. Kepler [5], in 1911, described a total of 151 cases of procidentia uteri in nulliparous women and classified the cases into two groups; those due to congenital defects occurring in the newborn period or at the time of puberty, and the second group were cases due to congenital defects occurring later in life. He also related mental defects to prolapsed uteri and described 38 cases where the patients were mentally retarded. Noyes [2], in 1927 reviewed extensively the anatomic dissections of several other authors and concluded that atrophy of the ligaments, connective tissue and muscles from defective innervation, secondary to spina bifida, contributed to the uterine prolapse Figure 3 and Figure 4. All the cases reported to that point in the literature, had a universally fatal outcome secondary to complications from meningomyelocele. |
|
|
PATHOPHYSIOLOGY OF PROLAPSE IN NEONATES AND YOUNG WOMEN
|
|
Some authors have studied the radiographic anatomy of normal infants and neonates with genital prolapse Figure 5 and Figure 6 [6,7]. In neonates and infants, the position of the pelvic organs is higher than in adults. For example, the urinary bladder is an intraabdominal organ with its space laying above the symphysis pubis; it does not reach its adult position in the pelvic floor until around 20 years of age. Zerin et al. [8] found an association between the descent of the bladder neck, denervation of the urethral sphincter, and the incidence of genital prolapse in children with myelodysplasia. Genital prolapse is present in 86 percent of infants with complete lower motor neuron denervation of the urethral sphincter, compared with only 13 percent when there is partial or lack of denervation. These studies support the reported observations where genital atrophy and prolapse are secondary to pelvic denervation from spinal defects. Noyes [2] also stressed the importance of spina bifida occulta as a cause for genital prolapse. They studied 28 cases of uterine prolapse and found that 28 percent of them showed spina bifida occulta whereas, an equal number of women without prolapse were used as controls, showing the condition only in 10 percent of cases. |
|
|
Patients with bladder extrophy also have associated genital prolapse [9]. These patients usually lack the lower inferior abdominal wall, the anterior portion of the bladder and the urethra. There is often an anterior displacement of the anus and deficient pelvic musculature resulting in rectal prolapse. The pelvic bones are widely separated anteriorly and the junction between the separated bony ends being filled with fibromuscular tissue. These patients usually develop prolapse from a huge defect in the anterior supporting structures of the pelvic floor. |
|
MANAGEMENT OF NEONATAL GENITAL PROLAPSE
|
|
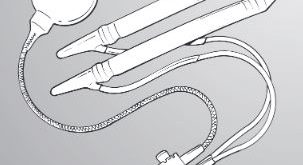
Digital reposition of the prolapse was the first reported intent for managing this condition. Noyes [2] and Ballantyne and Thomason [3] were the first to describe this mode of management, unfortunately babies died from meningitis in the first days of life Table 1. Fraser [10] was the first to describe the successful digital replacement of a prolapsed uterus in an otherwise normal newborn. More recently, Bayatpour et al. [11] reported the successful treatment of a child with no apparent neurologic anomalies by multiple digital reductions of the prolapse (the mother was trained to reduce the prolapse during diaper changes). When the tissues are edematous, the approach suggested by Ajabor and Okojie [12] with the application of hypertonic saline packs to the vulvar area, followed by digital repositioning of the mass with partial labial fusion with sutures would be appropriate. Dixon et al. [13] was the first to report the use of a pessary for the reduction of genital prolapse in a neonate. The pessary was made with a 1-inch, rolled, sterile Penrose drain with a 1-0 silk guy string attached Figure 7. Carpenter and Rock [16] reported an alternative approach by placing a nipple in the vagina, which was fixed with adhesive paper tape across the infant’s buttocks. |
|
|
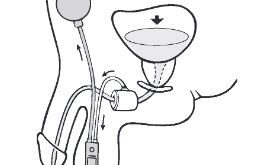
It seems, as evidenced in the literature, that simple digital replacements of the prolapsed genitalia or the use of small pessaries Figure 8 in normal neonates is successful. In the past, cervical amputation or hysterectomy were used as the ultimate treatment for genital prolapse in the neonatal period [2,10]. In patients with neurological impairment or myelomeningocele, nonsurgical treatment methods should also be attempted, given the good long-term outcomes obtained with conservative management and preservation of fertility. Surgical management is reserved until they reach an older age, if necessary. |
|
|
MANAGEMENT OF PROLAPSE IN THE YOUNG FEMALE
|
|
The surgical treatment of genital prolapse in young women, particularly for those who want to preserve their fertility, is a real challenge to the gynecologist. In general, there are techniques reported for both abdominal and vaginal approaches. The most common operation used in the past was the Manchester operation described in 1888 by Donald [1], which consisted in the plication of the uterosacral and cardinal ligaments with a partial amputation of the cervix. This operation had many drawbacks including reduction in fertility (pregnancy rates of 10-20 percent) [17], increased miscarriage rates, premature labor and dystocia leading to a cesarean section rate of 20 to 55 percent [18]. Enterocele formation and recurrence of the prolapse were frequent [19]. Description of more extensive techniques for the Manchester operation, like the one described by O’Leary and O’Leary [20], are also available Table 2, and they address the problem of recurrence by excising the enterocele sac and closing the cul-de-sac at a high level with a purse-string suture that included the uterosacral ligaments and the uterine serosa. |
|
|
More recent techniques have been described for the management of prolapse in young women. Durfee [22] and Nassar [23] advocated uterine suspension via Dacron tape or fascia passed through the round ligaments with attachment to the posterior border of the cervix. Unfortunately, these operations change the normal vaginal axis and allow the abdominal pressure to be transmitted directly to the cul-de-sac, potentiating enterocele formation. Chaudhuri [18] described both vaginal and abdominal internal oblique fascia sling operations, with good anatomical results and 66 percent pregnancy rates with only two recurrences. Other techniques for abdominal hysterosacropexy operations were described by Aboulghar and El-Kateb [21] and Dewhurst et al. [9] with similar results. |
|
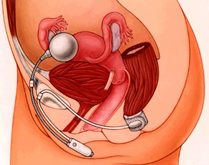
More recently, Richardson et al. [24] and Kovac and Cruikshank [25] advocated transvaginal sacrospinous fixation approaches for the correction of genital prolapse in young women. Both reports stressed that each individual defect of the pelvic floor had to be addressed in order to obtain optimal results. The report by Kovac and Cruikshank [25] was larger, and described 19 patients of whom 5 had a total of 6 deliveries with good outcomes and adequate anatomical support postdelivery. In that series, six patients were nulliparous, although none were pregnant at the time of publication. The sacrospinous fixation is simple with an average operating time of 15 minutes and minimal blood loss Figure 9 and Figure 10. This approach should be given serious consideration for the management of young patients with symptomatic uterine prolapse who wish to preserve their fertility, because it provides adequate anatomical restoration, avoiding an intraabdominal procedure that can potentially generate pelvic adhesions and enterocele formation. |
|
|
REFERENCES
|
|
1. Donald A. The operative treatment of prolapse of the uterus and vagina. J Obstet Gynecol Br Emp 1902;1:312-326. [Context Link] |
|
2. Noyes IH. Uterine prolapse associated with spina bifida in the newborn, with report of a case. Am J Obstet Gynecol 1927;13:209-213. Click here to check availability [Context Link] |
|
3. Ballantyne JW, Thomson J. Congenital prolapsus uteri with two illustrative cases. Am J Obstet 1897;35:161-175. [Context Link] |
|
4. Findley P. Prolapse of the uterus in nulliparous women. Am J Obstet Dif Wom 1917;75:12-21. [Context Link] |
|
5. Kepler CH. A consideration of complete procedentia in the nulliparous woman with special reference to lack of physical and mental development. Am J Obstet 1911;63:1007-1017. [Context Link] |
|
6. Siverman FN. The urinary tract and adrenal glands. In: Caffey J, ed. Pediatric X-ray Diagnosis, 7th ed. Chicago: Year Book Medical Publishers, Inc, 1978, p 880. [Context Link] |
|
7. Lee FA, McComb JG. Neurogenic perineal prolapse in neonates. Radiology 1983;148:433-435. Click here to check availability Bibliographic Links [Context Link] |
|
8. Zerin JM, Lebowitz RL, Bauer SB. Discent of the bladder neck: A urographic finding in denervation of the urethral sphincter in children with myelodysplasia. Radiology 1990;1974:833-836. [Context Link] |
|
9. Dewhurst J, Toplis PJ, Shepherd JH. Ivalon sponge hysterosacropexy for genital prolapse in patients with bladder extrophy. Br J Obstet Gynaecol 1980;87:67-69. Click here to check availability Bibliographic Links [Context Link] |
|
10. Fraser RD. A case of genital prolapse in a newborn baby. Br Med J 1961;5231:1011-1012. [Context Link] |
|
11. Bayatpour M, McCann J, Harris T et al. Neonatal genital prolapse. Pediatrics 1992;90:465-466. Click here to check availability Bibliographic Links [Context Link] |
|
12. Ajabor LN, Okojie SE. Genital prolapse in the newborn. Int Surg 1976;61:496-497. Click here to check availability Bibliographic Links [Context Link] |
|
13. Dixon RE, Acosta AA, Young RL. Penrose pessary management of neonatal genital prolapse. Am J Obstet Gynecol 1974; 119:855-857. Click here to check availability Bibliographic Links [Context Link] |
|
14. Shuwarger D, Young RL. Management of neonatal genital prolapse: Case reports and historic review. Obstet Gynecol 1985;66:61-63. Click here to check availability |
|
15. Johnson A, Ungar SW, Rogers BM. Uterine prolapse in the neonate. J Pediatr Surg 1984;19:210-211. Click here to check availability Bibliographic Links |
|
16. Carpenter SE, Rock JA. Procidentia in the newborn. Int J Gynecol Obstet 1987;25:151-153. Click here to check availability Bibliographic Links [Context Link] |
|
17. Fisher JJ. The effect of amputation of the cervix uteri upon subsequent partuition. Am J Obstet Gynecol 1951;62:644-648. Click here to check availability Bibliographic Links [Context Link] |
|
18. Chaudhuri SK. The place of sling operations in treating genital prolapse in young women. Int J Gynecol Obstet 1979;16:314-320. Click here to check availability Bibliographic Links [Context Link] |
|
19. Williams DFP. Surgical treatment of uterine prolapse in young women. Am J Obstet Gynecol 1966;95:967-971. Click here to check availability Bibliographic Links [Context Link] |
|
20. O’Leary JA, O’Leary JL. The extended Manchester operation. A review of 189 cases. Am J Obstet Gynecol 1970;107:546-550. [Context Link] |
|
21. Aboulghar MA, El-Kateb Y. Treatment of uterine prolapse in young women. Sacral cervicopexy by polyvinyl alcohol sponge. J Egypt Med Assoc 1978;61:127-134. Click here to check availability Bibliographic Links [Context Link] |
|
22. Durfee RB. Suspension operation for treatment of pelvic organ prolapse. Clin Obstet Gynecol 1966;9:1047. Ovid Full Text Bibliographic Links [Context Link] |
|
23. Nassar GF. Modified Williams-Richardson operation for uterine prolapse. Obstet Gynecol 1967;30:233. Click here to check availability Bibliographic Links [Context Link] |
|
24. Richardson DA, Scotti RJ, Ostergard DR. Surgical management of uterine prolapse in young women. J Rep Med 1989;34:388-391. [Context Link] |
|
25. Kovac SR, Cruikshank SH. Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in 5 of 19 patients. Am J Obstet Gynecol 1993;168:1778-1786. Click here to check availability Bibliographic Links [Context Link] |
|
|
|
 Figure 1 Figure 1 |
 Figure 2 Figure 2 |
 Figure 3 Figure 3 |
 Figure 4 Figure 4 |
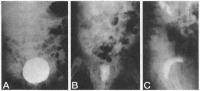 Figure 5 Figure 5 |
 Figure 6 Figure 6 |